When Cortisol Dips: Understanding Your Treatment Path
Why Cortisol Balance is Essential for Your Health

Low cortisol treatment involves replacing missing hormones through daily medication, typically using hydrocortisone or similar corticosteroids. Most people with adrenal insufficiency need:
- Daily hormone replacement: Hydrocortisone (15-25 mg/day) or cortisone acetate (20-35 mg/day) in divided doses
- Mineralocorticoid replacement: Fludrocortisone (50-100 cg/day) if you have primary adrenal insufficiency
- Stress dosing: Increased medication during illness, surgery, or physical stress
- Emergency preparedness: Carrying injectable hydrocortisone and wearing medical alert identification
- Regular monitoring: Annual checkups with an endocrinologist to adjust doses
Cortisol often gets labeled as the "stress hormone," but it does much more than help you handle pressure. This vital hormone, produced by your adrenal glands (small glands that sit on top of your kidneys), helps regulate metabolism, blood pressure, inflammation, and your response to stress. When your cortisol levels dip too lowa condition called adrenal insufficiencyeveryday tasks can feel overwhelming.
Low cortisol is not just about feeling tired. You might experience unexplained weight loss, constant fatigue, muscle weakness, dizziness when standing up, or intense cravings for salty foods. Some people notice darkening of their skin, while others struggle with nausea or mood changes. Because these symptoms develop gradually, they can be easy to dismiss until they become severe.
Primary adrenal insufficiency (Addison's disease) occurs when your adrenal glands are damaged and cannot produce enough cortisol. This affects about 1 in 100,000 people in the United States, and in the UK, autoimmune disorders account for most cases. Secondary adrenal insufficiency happens when your pituitary gland does not send the right signals to your adrenal glands, often due to long-term steroid use or pituitary problems.
The encouraging news is that low cortisol treatment is highly effective. With proper hormone replacement therapy, most people can return to their normal activities and quality of life. Treatment requires lifelong daily medication, but it is generally straightforward and manageable once you understand the basics.
I'm Dawn Dewane, a board-certified Family Nurse Practitioner with experience in managing complex medical conditions, including hormone optimization and low cortisol treatment protocols. My background in hematology/oncology and palliative care has given me a deep understanding of how hormone imbalances affect overall wellness, and I'm committed to helping you steer your treatment journey with confidence.
Uncovering the Problem: Symptoms, Causes, and Diagnosis
Understanding your body's signals is the first step toward effective low cortisol treatment. Here is how low cortisol can show up, what often causes it, and how medical professionals confirm the diagnosis.
Recognizing the Signs of Low Cortisol
When your adrenal glands do not produce enough cortisol, your body sends various signals. Symptoms often start subtly and worsen over time, so recognizing them early is important for timely diagnosis.
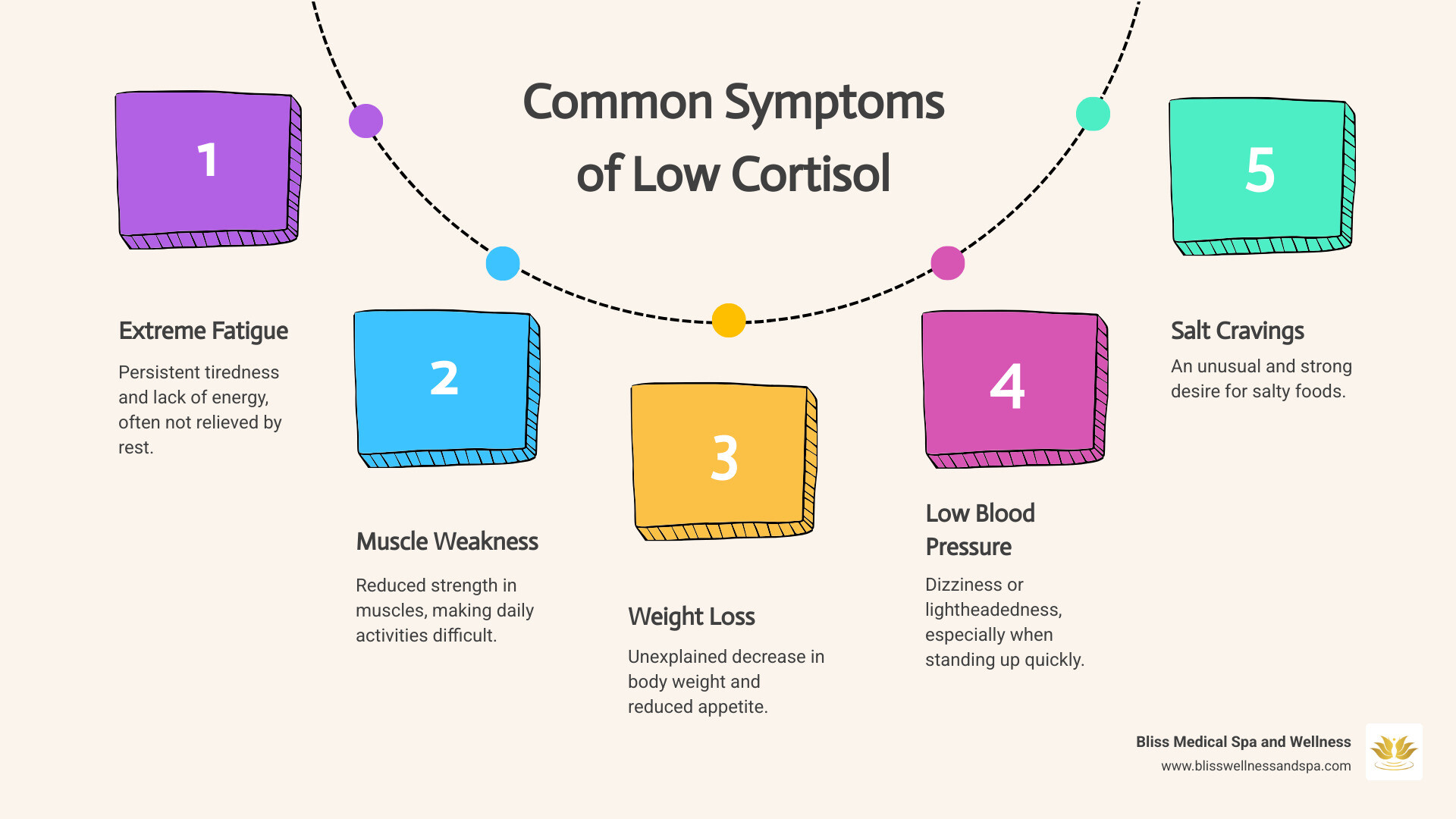
Common symptoms of low cortisol include:
- Persistent fatigue and weakness: Profound exhaustion that does not improve with rest, often accompanied by muscle weakness.
- Unexplained weight loss and decreased appetite: You may lose weight without trying and feel less interested in food.
- Low blood pressure (hypotension): Dizziness or lightheadedness, especially when standing up quickly (orthostatic hypotension).
- Intense salt cravings: A strong desire for salty foods as your body tries to compensate for electrolyte imbalances.
- Hyperpigmentation: Darkening of the skin, especially in sun-exposed areas, scars, skin creases (like knuckles or elbows), and sometimes on gums or inside the mouth. This is more common in primary adrenal insufficiency.
- Nausea, vomiting, and abdominal pain: Digestive issues can be frequent and distressing.
- Mood changes: Anxiety, depression, difficulty concentrating, or irritability.
- Hypoglycemia (low blood sugar): Particularly in children, this can show up as weakness, confusion, or even seizures.
These symptoms can significantly affect daily activities and quality of life.
What Causes Low Cortisol Levels?
Low cortisol, or adrenal insufficiency, can stem from several underlying causes, broadly grouped into primary and secondary forms.
Primary Adrenal Insufficiency (Addison's Disease): The adrenal glands themselves are damaged and cannot produce enough cortisol (and often aldosterone).
- Autoimmune attack: In the US, most Addison's disease cases are due to an autoimmune attack where the immune system destroys the adrenal cortex.
- Infections: Tuberculosis remains a major cause in some parts of the world. Other infections like HIV/AIDS and certain fungal infections can also damage the adrenal glands.
- Cancer: Spread of cancer to the adrenal glands can impair their function.
- Hemorrhage: Bleeding into the adrenal glands can cause acute adrenal failure.
- Surgical removal: If adrenal glands are surgically removed, hormone replacement is immediately necessary.
- Genetics: Certain genetic conditions, such as congenital adrenal hyperplasia, can lead to adrenal insufficiency from birth. Addison's disease is considered rare, affecting approximately 1 in 100,000 people in the United States.
Secondary Adrenal Insufficiency: The pituitary gland, located at the base of the brain, does not produce enough adrenocorticotropic hormone (ACTH). ACTH signals the adrenal glands to produce cortisol. Without sufficient ACTH, the adrenal glands produce less cortisol.
- Pituitary gland issues: Tumors, inflammation, or surgery on the pituitary gland can disrupt ACTH production.
- Long-term steroid use: The most common cause of secondary adrenal insufficiency is prolonged use of glucocorticoid medications (like prednisone). When stopped abruptly, the body's glands may not resume cortisol production quickly enough, leading to temporary or permanent insufficiency.
How Doctors Diagnose Adrenal Insufficiency
Accurate diagnosis is key for effective low cortisol treatment and involves a review of your medical history, a physical exam, and targeted tests.
Medical history and physical exam: Your provider will review your symptoms, how long they have been present, and any relevant medical conditions or medications. A physical exam may look for signs like hyperpigmentation or low blood pressure.
Blood tests:
- Cortisol levels: Blood samples are usually taken in the morning when cortisol levels are typically highest. A low morning cortisol level (for example, 40 nmol/L or 5 g/dL) can be a preliminary indicator.
- ACTH levels: High ACTH with low cortisol suggests primary adrenal insufficiency (the adrenals are not responding). Low ACTH with low cortisol points to secondary adrenal insufficiency.
- Electrolyte levels: Sodium and potassium levels are checked, as imbalances are common, especially in primary adrenal insufficiency where aldosterone is also affected.
ACTH stimulation test: This is considered the gold standard diagnostic tool for adrenal insufficiency.
- A synthetic form of ACTH (usually 250 cg) is administered.
- Blood cortisol levels are measured before and at specific intervals (typically 30 and 60 minutes) after the injection.
- If the adrenal glands are healthy, cortisol levels rise significantly. If they fail to respond adequately (for example, peak cortisol levels below 500 nmol/L or 18 g/dL), it confirms adrenal insufficiency.
- For a comprehensive understanding, you can refer to the Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline.
Insulin-induced hypoglycemia test: This test is used to assess secondary adrenal insufficiency, especially when pituitary function is in question. It involves inducing low blood sugar with insulin to monitor the cortisol response but is less common because it is complex and carries some risk.
Imaging tests:
- CT scan (computed tomography): A CT scan of the abdomen can visualize the adrenal glands to check for damage, tumors, or other abnormalities in cases of primary adrenal insufficiency.
- MRI (magnetic resonance imaging): An MRI of the brain may be performed if secondary adrenal insufficiency is suspected, to look for issues with the pituitary gland or hypothalamus.
This combination of history, exams, and testing helps identify the cause and severity of low cortisol and guides a personalized low cortisol treatment plan.
Your Core Low Cortisol Treatment Plan
Once adrenal insufficiency is diagnosed, the primary approach to low cortisol treatment is hormone replacement therapy. This does not cure the underlying problem, but it effectively manages symptoms and prevents serious complications. The goal is to replace missing hormones and mimic the body's natural rhythms as closely as possible.
Primary Low Cortisol Treatment: Glucocorticoid Replacement
Hormone replacement therapy for low cortisol primarily involves replacing glucocorticoids, with hydrocortisone being the most common choice. This is a lifelong commitment, but with the right dose and schedule, most people can lead full and active lives.
Key goals of treatment:
- Mimic circadian rhythm: Healthy adrenal glands release cortisol in a natural daily pattern, with higher levels in the morning and lower levels at night. Treatment aims to approximate this pattern to support energy, sleep, and overall function.
- Prevent adrenal crisis: Maintaining adequate cortisol levels is critical to prevent a life-threatening adrenal crisis, especially during times of stress.
- Avoid over-replacement: Under-replacement is dangerous, but too much glucocorticoid over time also carries risks, including:
- Obesity: Weight gain, particularly around the abdomen.
- Type 2 diabetes: Increased blood sugar levels.
- Osteoporosis: Weakening of bones, raising fracture risk.
- Hypertension: High blood pressure.
Finding the correct balance is key, and your healthcare provider will adjust dosages based on symptoms and clinical assessments.
The Role of Hydrocortisone
Hydrocortisone is the most widely prescribed medication for low cortisol treatment. It is chemically identical to the cortisol naturally produced by your body, making it a bioidentical hormone replacement.
- Dosing schedule: Hydrocortisone is typically taken two or three times a day by mouth. A common adult dose is 1525 mg/day, divided into doses. For example, a larger dose in the morning (for example, 10 mg), a smaller dose at midday (for example, 5 mg), and sometimes another small dose in the late afternoon or early evening (for example, 5 mg). This helps mimic your body's natural cortisol fluctuations.
- Why multiple doses? Because hydrocortisone has a short half-life, multiple daily doses are needed to maintain steady cortisol levels and prevent symptoms from returning between doses.
For more detailed information on hydrocortisone, you can refer to its dedicated page: More about hydrocortisone.
The Role of Fludrocortisone
For individuals with primary adrenal insufficiency (Addison's disease), the adrenal glands often fail to produce enough aldosterone, a hormone crucial for regulating sodium and fluid balance. This is where fludrocortisone comes in.
- Aldosterone replacement: Fludrocortisone acts as a synthetic replacement for aldosterone.
- Balances sodium and fluids: It helps your kidneys retain sodium and excrete potassium, which in turn supports blood pressure and fluid volume. This is vital for preventing dehydration and maintaining cardiovascular stability.
- Dosing: The typical starting dose for adults is 50100 cg per day, taken orally, usually once daily.
- When it is needed: Fludrocortisone is almost always prescribed for primary adrenal insufficiency. People with secondary adrenal insufficiency usually produce enough aldosterone on their own, so they typically do not need fludrocortisone.
You can learn more about fludrocortisone here: More about fludrocortisone.
Alternative Medications for Low Cortisol Treatment
While hydrocortisone is the most common and often preferred choice for low cortisol treatment, other corticosteroids like prednisone and dexamethasone can be used in selected situations or based on individual needs.
Here is a comparison of key medications:
| Medication | Chemical Structure | Half-Life/Duration of Action | Typical Dosing | Advantages | Disadvantages |
|---|---|---|---|---|---|
| Hydrocortisone | Identical to natural cortisol | Short (4-6 hours) | 2-3 times a day | Bioidentical, mimics natural rhythm well, easier to adjust for stress. | Requires multiple daily doses, can lead to fluctuating levels if not timed well. |
| Prednisone | Synthetic (similar to cortisol) | Medium (12-36 hours) | Once or twice a day (around 3-5 mg/d) | Longer-acting, better compliance, more stable cortisol curve, can be helpful if nausea or vomiting is an issue. | Historical concerns about side effects at higher doses (osteoporosis, lipid profile), less flexible for stress dosing. |
| Dexamethasone | Synthetic (very potent) | Long (36-72 hours) | Once a day (around 0.5 mg/d) | Very potent, long-acting. | Difficult to fine-tune dosage to mimic natural rhythm, higher risk of over-replacement side effects, generally not used for routine replacement. |
Prednisone: A synthetic corticosteroid that is more potent and longer-acting than hydrocortisone. Its longer half-life means it can often be taken once or twice daily (typically 35 mg/day), which may improve adherence. While older studies linked higher doses of prednisone to problems with bone density or lipid profile, newer research suggests that lower doses (for example, 1.84.2 mg daily) can be effective and safer for many patients with adrenal insufficiency. For more information, refer to Scientific research on prednisone.
Dexamethasone: A very potent, long-acting corticosteroid. Because of its potency and extended duration, it is challenging to adjust the dose to follow the body's natural cortisol rhythm without risking over-replacement. For this reason, it is less commonly prescribed for routine daily low cortisol treatment compared with hydrocortisone or prednisone. You can learn more about dexamethasone here: dexamethasone.
The choice of medication is a collaborative decision between you and your healthcare provider, based on your specific needs, lifestyle, and how your body responds to treatment.
Managing Low Cortisol in Special Situations
Living with low cortisol means being prepared for life's curveballs. Situations like illness, injury, surgery, or pregnancy place extra demands on your body and often require adjustments to your low cortisol treatment to prevent serious complications.
Adjusting Medication for Illness, Injury, or Surgery
Your body naturally produces more cortisol during times of stress to help you cope. With adrenal insufficiency, your body cannot do this on its own, so medication must be increased during these times. This is often called "stress dosing" or "sick day rules."
- General illness (fever, flu): For minor illnesses with fever (for example, 100.5F or higher), many specialists advise doubling your usual daily dose of glucocorticoids. For more severe infections, the dose may need to be tripled temporarily.
- Vomiting or diarrhea: If you have significant vomiting or diarrhea and cannot keep your oral medication down, this is a serious situation. Your body will not absorb the hormones it needs. If you vomit within 30 minutes of taking an oral dose, you should take that dose again. If vomiting recurs, it is critical to use an intramuscular hydrocortisone injection (if you have an emergency kit) and seek immediate care at the nearest emergency department.
- Injury: For significant injuries, such as a broken bone or a severe burn, a higher stress dose of corticosteroids, often given intravenously, may be needed right away.
- Surgery: Any surgery, especially with general anesthesia, is a major physical stressor. Your medical team can give intravenous corticosteroids (for example, hydrocortisone) before, during, and after the procedure. This "perioperative stress dosing" continues until you can safely resume oral medication. Doses are then tapered back to your usual maintenance dose as you recover.
Always consult your healthcare provider for specific instructions on adjusting medication in these situations. Acting promptly can prevent an adrenal crisis.
Navigating Pregnancy with Adrenal Insufficiency
Pregnancy is a time of major change for the body, and for individuals with adrenal insufficiency, it requires careful and proactive management of low cortisol treatment.
- Dose adjustments: Your maintenance dose of glucocorticoids often stays the same early in pregnancy, but an increase is commonly recommended in later pregnancy, especially the third trimester, as cortisol needs rise. Close monitoring by an endocrinologist and obstetrician is essential.
- Morning sickness challenges: If you have moderate to severe nausea and vomiting that keep you from holding down oral medication, corticosteroid injections (intramuscular hydrocortisone) may be necessary to maintain adequate hormone replacement. In severe cases, hospital care may be needed.
- Delivery management: Labor and delivery are significant stressors. They are managed similarly to surgery, with increased doses of corticosteroids, often given intravenously, during labor and in the immediate postpartum period.
- Post-delivery tapering: After delivery, corticosteroid doses are gradually reduced back to pre-pregnancy levels over days to weeks, depending on your recovery and clinical guidance.
With planning and communication, most people with adrenal insufficiency can have safe pregnancies and healthy babies.
What is an Adrenal Crisis and How is it Treated?
An adrenal crisis, also known as an Addisonian crisis, is a severe, life-threatening medical emergency that can occur if your body does not have enough cortisol during a period of extreme stress (such as severe illness, injury, or surgery) or if medication is missed or not adjusted appropriately.

Recognizing the signs: Symptoms can develop rapidly and may include:
- Sudden, severe pain in your lower back, abdomen, or legs
- Severe vomiting and diarrhea, leading to dehydration
- Extremely low blood pressure (shock)
- Loss of consciousness
- Confusion or disorientation
- Fever
- Hypoglycemia (low blood sugar)
- Rapid heart rate
Immediate action is critical: An adrenal crisis requires emergency medical attention. Call 911 (or your local emergency number) right away.
- Emergency hydrocortisone injection: If you or a trained family member or caregiver has an emergency hydrocortisone injection kit, administer 100 mg of hydrocortisone intramuscularly (into a large muscle like the thigh) without delay while waiting for emergency services.
- Intravenous fluids: Medical personnel will typically administer large amounts of intravenous (IV) saline solution, often with dextrose (sugar), to rehydrate you and stabilize blood pressure and blood sugar.
- Continuous corticosteroids: You will receive continuous intravenous corticosteroids until the crisis is controlled and you are stable enough to switch back to oral medication.
Understanding what an adrenal crisis is and how to respond can save lives. For further information, you can visit What is adrenal crisis (Addisons Disease Self-Help Group). Having an emergency kit and making sure those close to you know how to use it are central parts of a safe low cortisol treatment plan.
Living with Low Cortisol: Long-Term Management and Lifestyle
Managing low cortisol is a lifelong commitment to medication and self-care, but with the right strategies, you can do very well.
Your Long-Term Management Strategy
Living well with adrenal insufficiency involves consistency and preparedness.

Key components of long-term management include:
- Regular endocrinologist visits: Annual checkups with an endocrinologist or a provider experienced in hormone conditions help monitor your condition, review symptoms, and fine-tune your low cortisol treatment plan.
- Medical alert jewelry/card: Wear a medical alert bracelet or necklace and carry a steroid emergency card. This alerts emergency responders that you need corticosteroid treatment if you are unable to communicate.
- Carrying extra medication: Keep a sufficient supply of your medication at home and when you are away. When traveling, many experts recommend carrying double the amount you expect to need, along with a doctor's note, especially for air travel.
- Emergency injection kit: An emergency glucocorticoid injection kit (with injectable hydrocortisone, needles, and instructions) and training in its use are vital. Consider having a close family member trained as well.
- Educate loved ones: Inform family, friends, and close colleagues about your condition and how to help in an emergency, including recognizing signs of an adrenal crisis and administering an emergency injection.
How Doctors Monitor and Adjust Your Medication
Monitoring low cortisol treatment is mostly clinical, focusing on how you feel and how your body is functioning.
- Clinical assessment: Your provider will routinely ask about symptoms such as energy levels, sleep quality, mood, appetite, and any signs of under- or over-replacement.
- Signs of under-replacement: Persistent fatigue, muscle weakness, dizziness, salt cravings, nausea, weight loss.
- Signs of over-replacement: Weight gain, fluid retention, difficulty sleeping, increased appetite, mood changes, easy bruising.
- Blood pressure checks: Blood pressure is checked regularly, especially for individuals on fludrocortisone, to ensure fluid and electrolyte balance.
- Electrolyte levels: For patients on fludrocortisone, blood electrolytes (sodium and potassium) are checked periodically to help set the right dose.
- Avoiding routine hormone monitoring: Unlike some other hormone therapies, glucocorticoid replacement is usually not monitored by regular blood cortisol tests. Because cortisol levels naturally fluctuate and oral medications are absorbed at different rates, routine hormone testing can be misleading. How you feel and function is usually the best guide.
Based on these factors, your provider will adjust medication to ensure you are receiving the most appropriate low cortisol treatment for your needs.
Recommended Lifestyle Adjustments
While medication is the cornerstone of low cortisol treatment, lifestyle choices can support your overall health.
- Dietary sodium: If you are taking fludrocortisone, you may need to moderately increase your salt intake, especially if you experience salt cravings. This can be particularly important in hot weather or after vigorous exercise, when you lose more sodium through sweat. Always confirm any major dietary changes with your healthcare provider.
- Stress management techniques: Managing psychological stress remains important. Practices such as mindfulness, meditation, yoga, gentle breathing exercises, or spending time outdoors can help you cope with everyday stressors.
- Adequate sleep: Aim for regular, restorative sleep. A consistent sleep schedule and relaxing bedtime routine can support your overall well-being.
- Regular, moderate exercise: Physical activity supports heart health, mood, and bone strength. Choose moderate activities and listen to your body. During illness or high stress, adjust your activity level and follow your "sick day rules". For more insights on activity, you can explore this resource on exercise.
These lifestyle adjustments, combined with your prescribed medication and ongoing care, create a comprehensive plan for living well with low cortisol.
Conclusion: Taking Control of Your Cortisol Levels
Understanding and managing low cortisol is an ongoing process of self-awareness, medical care, and proactive planning. While a diagnosis of adrenal insufficiency can feel overwhelming at first, effective low cortisol treatment allows most people to regain energy, stabilize mood, and live actively.
Long-term success usually depends on:
- Taking daily hormone replacement as prescribed
- Following stress dosing and sick day rules in special situations
- Staying prepared for emergencies with medical alert identification and an injection kit
- Keeping regular follow-up appointments to adjust treatment as needed
At Bliss Wellness and Spa, we believe in a personalized approach to wellness. We understand that optimal health extends beyond treating symptoms; it includes supporting your body's intricate systems, including hormonal balance. Our team is dedicated to providing care that respects your individual needs and helps you feel confident in your treatment plan.
We are here to support you each step of the way as you steer low cortisol treatment and work toward your best possible well-being in Phoenix, AZ, and Glendale, AZ.
Take the next step in your wellness journey with hormone optimization
